5 Ordinary planar x-ray images are formed by placing a patient between an x-ray tube and an image receptor, usually a cassette containing an intensifying screen and a photographic film. The film is exposed by light emitted when transmitted x rays interact in the screen. The resulting "radiograph" is simply a static shadow image. Fluoroscopy is a variant of this procedure in which a fluorescent screen and an electronic image intensifier are used to form a continuous "moving picture,"
6 As the x rays traverse the patient, they can be absorbed, scattered or transmitted undisturbed to the receptor. The scattered x rays merely interfere with the information conveyed by the shadow pattern of transmitted rays. So a mechanical grid is inserted behind the patient to prevent most of the scattered x rays from reaching the cassette.
7 For a parallel, monoenergetic x-ray beam incident along the z axis, the distribution N(x,y) of transmitted x-ray photons at the image plane is given, in the absence of scattering, by
No A∫e -µ(z) d z
where the line integral is taken over all tissues along the unscattered photon trajectory to the point (x,y) on the plane, µ is the linear attenuation coefficient for x rays of the tissue
encountered at (x, y, z) and A is the x-ray energy absorption coefficient of the
intensifying screen. The distribution of x rays absorbed in the screen thus
forms a two-dimensional projection image of the transmission of x rays through
the three-dimensional volume of tissue exposed to the x-ray beam.
8 The linear attenuation coefficient µ is in fact the sum of the coefficients for
various types of x-ray interactions. For the range of x-ray energies employed in medical imaging, two kinds of interactions predominate: the photoelectric effect, described by the linear attenuation coefficient τ, and Compton scattering, described by the linear attenuation coefficient σ. Thus µ = τ + σ. Figure 1 shows the x-ray energy dependence of these coefficients in humansoft tissue.
9 The photoelectric coefficient increases with atomic number Z like Z3, principally because x rays interact photoelectrically with the inner, tightly bound electrons of an atom. The Compton coefficient, by contrast, is relatively independent of the atomic number of the tissue atoms, because x rays Compton scatter almost exclusively off the outer, loosely bound atomic electrons. Both coefficients increase linearly with the tissue density. To achieve contrast between soft tissues that differ only slightly in Z, one must use low-energy x rays, because they interact predominantly by the photoelectric effect. An example is mammography, which employs x rays in the range of 15-30 keV. For chest x rays, which involve tissues of greater intrinsiccontrast, clinicians use x rays with energies ranging from 50 to 150 keV.
10 X-ray images represent a compromise among four kinds of resolution: spatial, contrast, temporal and statistical. Spatial resolution is related to the geometry of the image-forming process and the resolving capacity of the intensifying screen. Contrast resolution is affected by the attenuation characteristics of the various tissues, the x-ray energy and the glare from scattered x rays that cannot be kept from the screen. Temporal resolution refers to the blurring caused by the patient's movement during exposure. Statistical resolution is related to the number of x ray photons absorbed in the screen to produce the image; the more photons, the less statistical noise.
11 Unfortunately, improving any one of these resolution factors generally degrades one or more of the others. The compromise among them represents a balance such that no single factor dominates the degradation of the image.
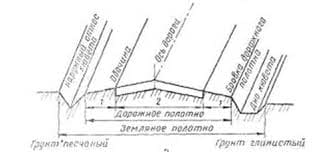
Sectional imaging
12 A fundamental limitation in conventional planar x-ray imaging is the projection of the three-dimensional distribution of attenuation coefficients as a shadow onto a two-dimensional detector. This projection obviously discards much information about tissue variation along the beam direction. For many years techniques of analog tomography were used in attempts to overcome this limitation. But they were restricted to certain specific applications, and the images were difficult to interpret.
13 A major breakthrough was achieved in 1972 with the introduction of x-ray transmission computed tomography (often abbreviated as CT or CAT). This technique was brought to clinical medicine through the efforts of Godfrey Hounsfield and Allan Cormack, who shared the 1979 Nobel Prize in medicine. Several other investigators contributed significantly to the foundations of this important x-ray imaging technique.
14 To understand the principles of CT scanning, consider a highly collimated x-ray pencil beam in the plane of a slice of the body only a few millimeters thick. X rays transmitted all the way through the slice are measured with a collimated detector on the opposite side of the patient. The signal from the x-ray detector (an ionization chamber or a scintillation detector) is converted to digital output. The tight collimation of source and detector prevents scattered radiation from degrading image contrast. The number of x-ray photons recorded by the detector at one position constitutes a single pencil-beam projection of x-ray transmission data at a specific angle through the tissue slice. This process is repeated many times at slightly different angles to create a set of multiple projections of the entire tissue slice. (See figure 2a.)
15 If x-ray projection data are collected at a sufficient number of angles, a matrix of values of the attenuation coefficient µ. for different δx δy cells can be calculated by a simple back-projection technique, thus yielding the two-dimensional distribution µ(x, y) over the whole tissue slice. By displaying the variation of the attenuation coefficient pictorially in shades of gray, one creates an image that shows the various anatomical features of the tissue slice.
Digital imaging
16 The combination of intensifying screen and photographic film has many advantages for capturing and recording x-ray images. It is simple, portable and inexpensive, and it yields excellent spatial resolution. But it is limited to a narrow range of acceptable exposures and offers little flexibility for image processing or data compression. Film images are bulky to store, and they must be transported physically from one location to another.
17 Digital imaging methods overcome these limitations, but currently they are more expensive and more complex. Digital methods employ a variety of approaches for x-ray detection and measurement: fluorescent crystals with photomultipliers, semiconductor detectors, channel electron multipliers and photo stimulatable phosphors with laser-scanning readout. As these techniques evolve, medical imaging is becoming increasingly reliant on digital technologies. It is likely that clinical imaging will be entirely digital in the not-too-distant future.
18 In a digital planar radiographic unit, as shown in figure 3, the x-ray source and receptor are computer-controlled to provide digital images that can be displayed in real time on video screens. Digital images can be stored on magnetic media or optical disk, and a film-writing device may be used to produce permanent analog copies of the images, if they are wanted. Digital image storage and display are used routinely in x-ray CT and magnetic resonance imaging. The convenience and utility of digital technology is encouraging its adoption for other imaging modalities.
19 Two types of image receptors are used in digital radiography. One type records the entire image simultaneously; the other acquires a complete image by scanning the x-ray beam and receptor in synchrony across the patient, a technique known as scanned-projection radiography. Various data acquisition methods are available, including the use of image intensifiers, ionographic chambers, solid-state detector arrays and stimulated-luminescence plates. Commercially available stimulated-luminescence plates employ a phosphor that absorbs x-ray photons and reradiates their energy in the visible when scanned with a laser beam. The emitted light is detected by a photomultiplier tube and digitized with an 8- or 16-bit analog-to-digital converter. The digitized image is displayed on a video monitor and stored.
 Figure 2
Figure 2
Evolution of geometries of x-ray CT scanners. A: First-generation scanner, in which the pencil x-ray beam is both translated and rotated to cover the body being imaged; the moveable detector is shown in green. B: Second-generation scanner, with a diverging fan beam and detector array that are translated and rotated. C: Third-generation scanner,with a fan-beam source that rotates around the body together with its detector bank. D: Fourth-generation detector, with a rotating fan-beam source and a stationary ring of detectors.
20 Scanning systems for digital radiography have the advantage of excellent rejection of scattered radiation by means of tight collimation of the x-ray beam near the source and the detector. The beam may be scanned as a point or line across the patient. Line scanning requires several seconds to compile data for a single image. But the exposure of any particular region of tissue is so brief that the image suffers little motion blurring. With point scanning, one can varythe dwell time for different tissue locations so that the detector sees a constant photon flux, more or less. This technique, called scan-equalization radiography, is designed to control statistical unsharpness.
21 Digital images offer numerous advantages over screen and film radiography. The data can be compressed for rapid electronic transmission. They require less storage space, and copies can be presented for viewing without risk of misplacing the original. The acquisition of digital x-ray images sometimes requires less radiation exposure than does conventional analog imaging. Also, computer subtraction of images taken at different times can quickly reveal changes in a patient's state.
22 Digital techniques have the potential of moving medical imaging toward an on-line, real-time diagnostic regime that promises more efficient and responsive medical care.
Remote transmission, called teleradiology, is already important in military medicine as a means of providing expert consultation on battlefield injuries.
X-ray therapy
23 Very soon after Rontgen's discovery, x rays began to be used to treat cancer and a variety of other illnesses. For several decades these treatments were undertaken with x rays produced at tube potentials of a few hundred volts. Although such treatments helped many thousands of patients, some indiviuals experienced adverse side effects caused by the tissue-destroying properties of x rays. The x rays delivered the highest dose to the patient's skin, and the degree of skin reddening (erythema) was used as a measure of how well the patient was tolerating radiation treatment.
24 After World War II, radioisotopes from nuclear reactors became available. One such isotope, cobalt-60, had excellent attributes as a so-called teletherapy source for external-beam treatment of tumors deep inside the body. Its energetic gamma rays (1.17 and 1.33 MeV) were highly penetrating andthey delivered their maximum dose a few millimeters below the skin surface. With the skin surface spared, patients could tolerate greater therapeutic doses. This was a major clinical advance, but it deprived the clinician of skin response as an indicator of the patient's dose tolerance.
25 In place of skin response, clinicians and physicists combined detailed measurements of radiation-beam characteristics with calculations of dose distributions to develop treatment plans. At first these plans were compiled manually. Soon, however, computers became essential for handling the large data volume and meeting the need to generate individualized plans. All this requires as much physics as medicine. So medical physicists quickly became pivotal members of radiation therapy teams.
26 Cobalt-60 does have its disadvantages. Dose rates are quite limited and the beam margins are rather un-sharp. In the 1960s 60Co units began to be replaced by linear accelerators designed to produce intense, sharply defined beams of high-energy (a few MeV) x rays. The development of the standing- wave, side-coupled linear accelerator was a major design breakthrough. It gave clinicians a compact high-energy accelerator ideal for use in radiation therapy where space is limited and positional flexibility is desirable. Linear accelerators have now replaced 60Co units for almost all external-beam radiation treatment. In addition to x rays, these units provide electron beams for treating relatively superficial tumors. Linear accelerators require extensive dosimetry and quality management, further enhancing the need for oversight by medical physicists.
27 For treatment of cancers in accessible organs and body cavities, implanted radioactive sources have competed over the years with external radiation sources. Implanted sources are the preferred treatment for cancers in specific organs, Generally they emit gamma rays, but one popular source (iodine-125) also emits characteristic x rays. The use of implanted radioactive sources is an elaborate process requiring care to protect the patient and attending personnel from excessive exposure. Detailed procedures and computations are used to ensure proper source placement and adequate radiation-dose delivery. This requires the involvement of medical physicists, working collaboratively with clinicians to meet the exacting demands of optimal patient care.
Treatment planning
28 The successful treatment of cancer with x rays requires that the tumor and all of its microscopic extensions into normal tissue receive a radiation dose sufficient to kill the cancer cells. At the same time one must avoid the serious complications that result from overexposing nearby normal tissue.
29 The patient's survival probability as a function of radiation dose is the blue curve in figure 4. If the dose is low, the tumor is likely to recur. At high doses, on the other hand, the therapy itself is likely to cause unacceptable complications. Between these extremes the physician seeks to maximize the patient's survival of both the cancer and the treatment. But if the patient's discomfort is too severe at the radiation dose Dopt that optimizes the product of the two competing factors, the physician may choose a somewhat lower dosage.
30 Radiation dose optimization in cancer therapy demands careful delineation of the margins of the tumor. That requires good medical imaging. The use of planar radiographs had several limitations. It was difficult to visualize the tumor clearly, and difficult to transcribe the radiographic information to the cross-sectional plane used to design the treatment plan.
31 CT and, more recently, magnetic resonance imaging have largely overcome these difficulties. Many treatment centers have a CT unit dedicated to treatment planning and monitoring. The images not only provide a cross-sectional representation of the patient's internal anatomy, but also yield an accurate representation of the body contour and, often, excellent visibility of the tumor and surrounding normal tissues. Because the data are digital, they can be entered directly into the treatment-planning computer so that proposed treatment plans can be superimposed directly onto the CT images. Then the plan can be implemented on the treatment machine.
32 For such a process to succeed, however, the geometry used to acquire the CT data must correspond precisely to the patient's setup for each of the subsequent treatments. That is accomplished by laser alignment employing reference marks on the patient, and then periodic verification with a treatment simulator constructed to reproduce the proper geometry. The medical physicist must closely monitor the alignment of radiation-dose delivery with the tomographic input data and the computed treatment plan.
|
|
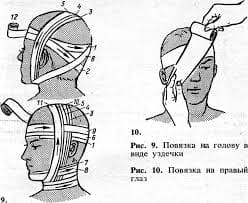
Figure 3
Digital radiographic system creates digital x-ray images that can be displayed in real time or stored. X rays that traverse the patient unscattered are recorded at the digital receptor screen and the data are passed on for processing and display. Scattered x-ray photons are kept from the receptor screen by an antiscatter grid.
Tomographic therapy
33 Most applications of x-ray CT information to radiation treatment planning rely on a commercial CT scanner and various external techniques to maintain the alignment of the scanner and the accelerator with the treatment plan. But a number of medical physicists have built CT scanners on treatment-simulator gantries. Usually such units compile image projections by digitizing the output from a television camera that monitors the transmitted x-ray intensity imaged on an image-intensifier screen. Although these units do not provide resolution comparable to that from a diagnostic CT scanner, they duplicate the treatment geometry and yield images good enough for treatment planning.
34 The images from a CT unit are gray-scale representations of the matrix of attenuation-coefficient values across a planar section through the tumor. If the matrix could be measured at the x-ray energies used in treatment, then the dose distribution could be corrected for the presence of nonhomogeneous structures in the irradiated tissue, and patient alignment could be monitored during the treatment. Several groups have successfully developed detectors and computer algorithms to accomplish these objectives with megavolt treatment machines.
35 Most radiation treatments nowadays involve the use of multiple fixed radiation fields converging on the tumor from different angles. Thus the dose can be concentrated in the tumor while much lower doses are delivered to surrounding normal tissues. In many cases one can get an even better dose distribution by continually rotating the gantry of the x-ray accelerator around the patient during treatment so that only the tumor is constantly in the path of the beam. But this rotating-beam therapy is complicated by the fact that malignant tumors are notoriously asymmetrical. Therefore the size of the radiation field has to be varied continuously as the beam direction through the tumor changes. The dose distributions could be improved even further by also varying the beam intensity during the rotation. This approach, called conformal therapy, is being pursued in several centers in the US and overseas. It requires detailed three-dimensional knowledge of the anatomy of the irradiated tissue. It also requires exquisite computerized positioning control of the accelerator, the gantry and the patient's couch.
36 A significant advance in conformal therapy would be the convergence of CT and megavoltage therapy in a single gantry, so that tomographic images could monitor alignment and dose distribution continually during treatment. This hybrid approach remains to be developed in full. It presents a number of challenges, but the potential benefit is considerable.
37 The modern uses of x rays for clinical imaging and therapy are a prime example of “high-tech” medicine.They illustrate the contributions of physicists working with physicians to improve diagnosis and treatment. Much remains to be done, especially in refining the growing convergence of imaging with therapeutic irradiation. Medical physics will continue to other physicists many opportunities to apply their special knowledge to the healing arts.
IV. Reading for General Understanding.
1. Check the comprehension of the text “X-rays in Medicine” by choosing the answer,
which you think, is correct.
1) Half a million cancer patients each year receive x-ray treatments, about half of them
for curative purposes and the rest for pain relief.
a) yes,it’s true
b) it is mostly true. I think it’s more the than half a million.
c) No, it is not so. X-ray treatments are used only for pain relief.
2) The development of noninvasive imaging techniques of various kinds started in
Röntgen’s physics laboratory a hundred years ago.
a) I think this development started more than a hundred years ago.
b) No it’s not true. At that time there was imaging with radio-isotopes.
c) Yes, that’s right.
3) A major breakthrough was achieved in 1972 with the introduction of law-energy x-rays.
a) You are quite right.
b) No it is not so. The major breakthrough was achieved in 1982.
c) You are mistaken. The major breakthrough was achieved in 1972 with the
d) introduction of x-ray transmission computed tomography.
4) Film images are bulky to store and they must be transported physically from one
location to another.
a) You are mistaken. Film images are quite small and they are easy to store.
b) No, you are not right. Film images are bulky to store, but they are transmitted
by cables.
c) You are right. Film images are transported physically and they are bulky to store.
5) The beam may be scanned as a point or line across the patient.
a) The beam is not scanned. It is fixed.
b) The beam may be scanned under the patient.
c) The beam may be scanned across the patient as a point or line.
6) Dose rates are quite limited and the beam margins are rather unsharp.
a) You are mistaken. Dose rates are limitless and the beam margins are rather
unsharp.
b) You are not right either. Dose rates are quite limited and the beam margins are
rather sharp.
c) I think, I am right. Dose rates are limited and the beam margins are rather unsharp.
7) The use of implanted radioactive sources is an elaborate process requiring care
to protect the patient and attending personnel from excessive exposure
a) You are wrong. The use of implanted radioactive sources doesn’t require care
b) to protect the patient and attending personnel.
.
c) The use of implanted radioactive sources is a simple process that requires to
protect neither the patient nor attending personnel.
d) The use of implanted radioactive sources requires care to protect the attending
personnel and patient and it is not a simple process.
8) The use of planar radiographs had several limitations.
a) You are wrong. The use of planar radiographs had no limitations.
b) You are mistaken. It is the use of x-ray technique that has several
limitations.
c)You are quite right. It is the use of planar radiographs that has several
limitations.
9) Because the data are digital they can be entered directly into the treatment-
planning computer
a) Digital data cannot be entered directly into the treatment-planning computer
because they have several limitations.
b) Only digital data can be entered directly into the treatment-planning computer.
c) It is analog data that can be entered directly into the treatment-planning computer.
10)Therefore the size of the radiation field has to be varied continuously as the
beam direction through the tumor changes.
a) You are quite right. Since the beam direction through the tumor changes,
the size of the radiation field must be varied continuously.
b) You are mistaken. As the beam direction through the tumor does
not change, there is no need to vary continuously the size of the radiation field.
c) You are wrong. As the beam direction through the field remains fixed
therefore the size of the radiation field has to be varied continuously.
2. Pick out from the text all the word combinations with the following words (terms)
and give their Russian equivalents.
- image - effect
- imaging - radiation
- resolution - therapy
- scattering - accelerator
V. Reading for Detail and Language Study.
1.Find in the text “X-rays in Medicine” the English equivalents for the following
phrases: “Sectional imaging”
- методы аналоговой томографии
- трёхмерное распределение
- конкретные области применения
- преодолеть это ограничение
- предача данных под определённым углом
- основной прорыв
- сигнал с детектора х лучей
- коэффициент затухания
“Digital Imaging”
- фотографическая плёнка
- преодолеть эти ограничения
- цифровые технологии
- различные методы сбора данных
- обработка изображений
- постоянный поток фотонов
- цифровые методы
- режим диагностики в реальном времени
- дистанционная передача изображения
“X-ray Therapy”
- лечение
- кожа пациента
- гамма лучи
- линейный ускоритель стоячей волны
- свойства разрушения тканей
- лучевая терапия
- вживлённый радиоактивный источник
“Treatment Planning”
- доза облучения
- магнитный резонанс
- недопустимые осложнения
- плоскость поперечного сечения
- планы лечения
- ЭВМ, планирующая лечение
- аппарат для лечения
- опорные метки на пациенте
" Tomographic Therapy”
-разрешающая способность
-интенсивность луча во время вращения
-на пути луча
-распределение дозы облучения
- входные данные для томограммы
2. Explain the meaning of the following words and expressions.
- Noninvasive imaging techniques.
- X-ray energy
- Planar x-ray images
- Implanted radioactive sources
- CT scanner
- High-Tech medicine
3. Translate the text “Tomographic therapy” in written form.
VI. Oral Practice
1. Answer the questions on the text “X-rays in Medicine”
a) In what way are ordinary planar x ray images formed?
b) What happens to x rays while traversing the patient?
c) What forms a two-dimensional; projection of the transmission of x rays and when?
d) What kind of interactions predominates in x ray energies employed in medical imaging.
e) What energies do clinicians use for chest x rays.
f) Name different kinds of resolution and describe each of them.
2. Speak on the following:
a) Disadvantages of Cobalt-60.
b) Linear accelerators used for tumor treatment.
c) Implanted radioactive sources.
 2018-02-14
2018-02-14 270
270