A hallmark feature of OA pathology is the higher rate of cartilage degradation than cartilage synthesis, leading to chronic cartilage loss. Cartilage, composed of chondrocytes and the extracellular matrix (ECM), is a connective tissue possessing unique biological and mechanical properties which supports its load-bearing function [20]. The dry weight of cartilage is mainly made of type II collagen and some type I, along with certain amount of proteoglycans and integral proteins.
Fragments of these components generated during cartilage degeneration can be released into the bloodstream, synovial fluid, and urine and therefore be utilized as biomarkers [21].
C-Telopeptides of Type II Collagen
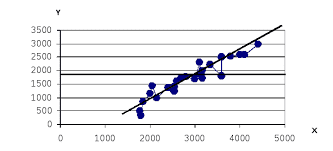
Since type II collagen is the major collagen type and most abundant protein in cartilage, C-terminal telopeptides of type II collagen (CTX-II), a catabolic product of type II collagen, has become the widely accepted biomarker for assessing collagen breakdown [18]. Urinary levels of CTX-II (uCTX-II) have been used as a marker for cartilage metabolism, disease severity, and monitoring drug response in OA patients [12]. Reijman et al. studied the association between the concentration of uCTX-II and the prevalence and progression of radiographic OA of the knee and hip.
They found that subjects with a uCTX-II level in the highest quartile had a 4.2-fold increased risk of having radiographic knee or hip OA, compared with subjects with a uCTX-II level in the lowest quartile. Furthermore, subjects with an uCTX-II level in the highest quartile had a 6.0-fold increased risk for progression of radiographic knee OA at the knee and an 8.4-fold increased risk for progression of radiographic hip OA. In addition to its strong correlation with radiographic OA, another advantage of uCTXII or serum CTX-II is that it is noninvasive. However, as collagen type II breakdown correlates with radiographic features of OA, the use of uCTX-II as a pre-radiographic diagnostic biomarker is limited.
Cartilage Oligomeric Matrix Protein
Cartilage oligomeric matrix protein (COMP) is a structural glycoprotein binding to and stabilizing type I, II, and IX collagen fibers, fibronectin, and aggrecan [10].
COMP has been considered as an OA biomarker and has been tested in OA diagnosis, prognosis, and therapeutic intervention. Many large population studies have shown that serum COMP (sCOMP) levels correlated with cartilage degradation and disease severity. In the Johnston County OA Project involving 143 patients with radiographic knee OA and 148 healthy controls, a significant elevation of sCOMP levels were detected in the OA group compared to controls. Moreover, sCOMP levels were upregulated with knee OA K-L grade and the number of joints involved [11]. Sharif et al. suggested the use of sCOMP levels to predict OA progression. In this longitudinal study lasting 5 years, 115 patients with OA were grouped as nonprogressors and progressors defined by either a reduction in the tibiofemoral joint space width by at least 2 mm or total knee arthroplasty at follow-up. They found that the chance to have radiographic OA progression was increased by 15 % with every 1 unit increase in sCOMP levels [14]. The existence of COMP fragments and their release into the culture medium were also confirmed recently which may provide complement to total COMP in use as biomarkers [11].
Hyaluronic Acid
Hyaluronic acid (HA) is a common component of most connective tissues, as well as a principal component of the synovial fluid. During the degenerative process, HA is secreted by the synovium and cartilage. Serum levels of HA were proposed to be a marker to predict the progression of knee OA [8]. OA patients had increased serum HA (sHA), and patients with higher initial sHA values displayed a more rapid progression of the disease. More recent studies also suggested that sHA can be available as a burden of disease marker for patients with radiographic or severe OA. The major problem associated with HA as an OA biomarker is its specificity and sensitivity, as HA is ubiquitously present in all connective tissues and tends to be affected by physical activities and food intake [ 5].
Despite the existence of multiple catabolic biomarkers in research, currently, there is no single biomarker validated for clinical use for OA. Given the unique advantages and disadvantages of these biomarkers, combined use of different biomarkers might be of benefit in the future. Also, majority of the abovementioned biomarkers are systemic, for example, from serum or urine, and their concentrations are subject to systemic conditions or illnesses. Therefore, obtaining local biomarkers from synovial fluid may provide more specificity and sensitivity. Moreover, local biomarkers would ensure the ability to detect OA in a particular joint [7].
 2017-10-31
2017-10-31 151
151